Patient Case Navigator: Major Depressive Disorder

Introduction
Learning Objectives
Learning Objectives
- How to perform a structured psychiatric interview
- Standardized psychiatric rating scales appropriate for patients with depressive symptoms
- Common barriers to adequate treatment response
- How to assess and monitor patients for treatment side effects and adequate treatment response
Watch the video:
History and Examination
Medical History
Examination
History of Present Illness
Eric is a 60-year-old man who presents to his primary care nurse practitioner, Tina, with irritability, excessive sleeping, and a lack of interest in his usual hobbies, such as attending baseball games and going to the movies with his wife. He also has been spending much time at home alone, watching television, rather than spending time with his friends or wife, as he usually does. Eric recently retired from his job as a general contractor remodeling people’s kitchens and bathrooms. He enjoyed his job very much and felt a sense of pride in helping people make their homes more functional and attractive. However, his job was very physical, and at times stressful, so Eric felt it was time to retire and find something new with which to occupy his time.
Medical History
Eric was diagnosed with hypothyroidism 5 years ago and has been on medication ever since. Annual lab tests indicate his thyroid levels have remained within the normal range for the past few years. He also has mild hypertension, which is well-controlled at an adequate dose.
Psychosocial History
Eric reports that he has several close friends and that he got along well with people at work. He denies a history of substance misuse and reports that he occasionally drinks a glass of wine with dinner. He does not smoke. Eric describes his marriage as “very good.” He is also close with his adult daughter and enjoys spending time with his 2 grandchildren.
At age 33, Eric experienced a period of depressed mood after losing his job. During that time, he had problems getting out of bed in the morning because he felt hopeless and sad, stopped socializing with friends, and lost about 4 lbs of body weight in 4 weeks without intentionally dieting. He sought treatment from his primary care physician, who referred him to a psychiatrist for medication and a psychologist for outpatient cognitive-behavioral therapy (CBT). Eric worked with his psychiatrist and tried 4 different selective serotonin reuptake inhibitors (SSRIs) before he ultimately found one that seemed to work for him. He and his psychiatrist decided together that he could stop taking the medication after 1 year because his mood had improved and stabilized. He saw his therapist once weekly for approximately 2.5 years and reports that CBT also helped improve his mood and functioning.
Family History
Eric reports that, throughout his life, his mother had “very low periods” when she seemed extremely sad and had trouble functioning. However, she never sought treatment for these episodes.
Eric’s physical examination indicates he is generally healthy for his age. His vital signs are all within the normal range, and the mental status examination indicates he is fully oriented and alert. Eric’s appearance is that of an older man. His affect is flat, and he has trouble making eye contact, often staring at the floor instead.
Watch the video:
Patient Interview
Quiz #1: Initial Presentation and Diagnosis
DSM-5 Diagnostic Criteria for MDD
MDE Diagnostic Criteria
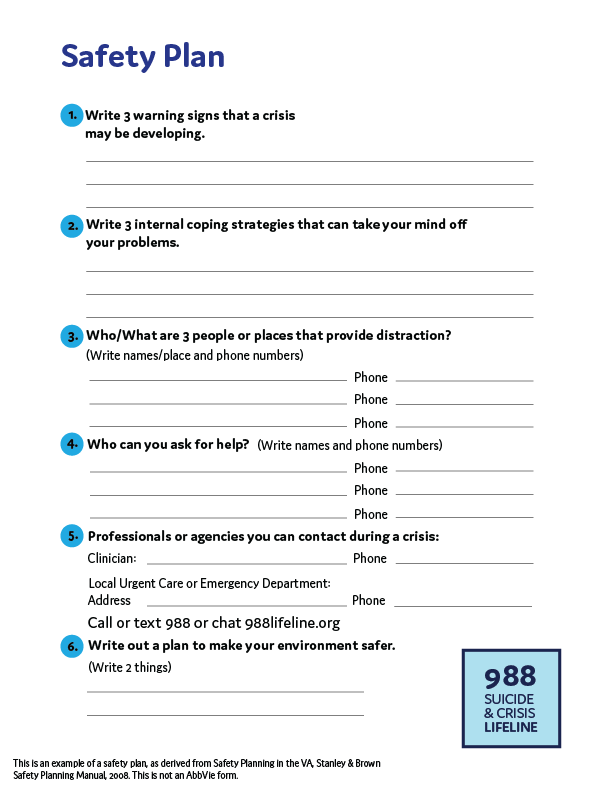
Safety Plan
Key Points
Major Depressive Episode (MDE)
A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous function; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
- Depressed mood most of the day, nearly every day, as indicated by either subjective report or observation made by others
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
- Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day
- Insomnia or hypersomnia nearly every day
- Psychomotor agitation or retardation nearly every day
- Fatigue or loss of energy nearly every day
- Feelings of worthlessness or excessive or inappropriate guilt nearly every day
- Diminished ability to think or concentrate, or indecisiveness, nearly every day
- Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide
B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of function
C. The episode is not attributable to the physiological effects of a substance or another medical condition
Diagnostic and Statistical Manual of Mental Disorders. 5th ed.American Psychiatric Association; 2013.
Key Points
- It is important to thoroughly review each of these 9 symptoms with your patients when assessing them for MDD.
- Clinical rating scales can help identify which patients require more in-depth screening for depression.
Watch the video:
Quiz #2: DSM-5 Diagnostic Criteria for MDD
Scales for MDD
PHQ-9
PHQ-9 Scale Scoring
QIDS
QIDS Scale Scoring
Patient Health Questionnaire-9 (PHQ-9)
| Over the last 2 weeks, how often have you been bothered by any of the following problems? (Use "✓" to indicate your answer) | Not at all | Several days | More than half the days | Nearly every day |
|---|---|---|---|---|
| 1. Little interest or pleasure in doing things | 0 | 1 | 2 | 3 |
| 2. Feeling down, depressed, or hopeless | 0 | 1 | 2 | 3 |
| 3. Trouble falling or staying asleep, or sleeping too much | 0 | 1 | 2 | 3 |
| 4. Feeling tired or having little energy | 0 | 1 | 2 | 3 |
| 5. Poor appetite or overeating | 0 | 1 | 2 | 3 |
| 6. Feeling bad about yourself - or that you are a failure or have let yourself or your family down | 0 | 1 | 2 | 3 |
| 7. Trouble concentrating on things, such as reading the newspaper or watching television | 0 | 1 | 2 | 3 |
| 8. Moving or speaking slowly that other people could have noticed? Or the opposite - being so fidgety or restless that you have been moving around a lot more that usual |
0 | 1 | 2 | 3 |
| 9. Thoughts that you would be better off dead or of hurting yourself in some way | 0 | 1 | 2 | 3 |
| For Office Coding: | 0 | + | + | + |
| = | Total Score: | _____ |
| If you checked off any problems, how difficult have those problems made it for you to do your work, take care of things at home, or get along with other people? | |||
|---|---|---|---|
| Not difficult at all | Somewhat difficult | Very difficult | Extremely difficult |
This scale was developed by Drs Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke, and colleagues with an educational grant from Pfizer inc. No permission required.
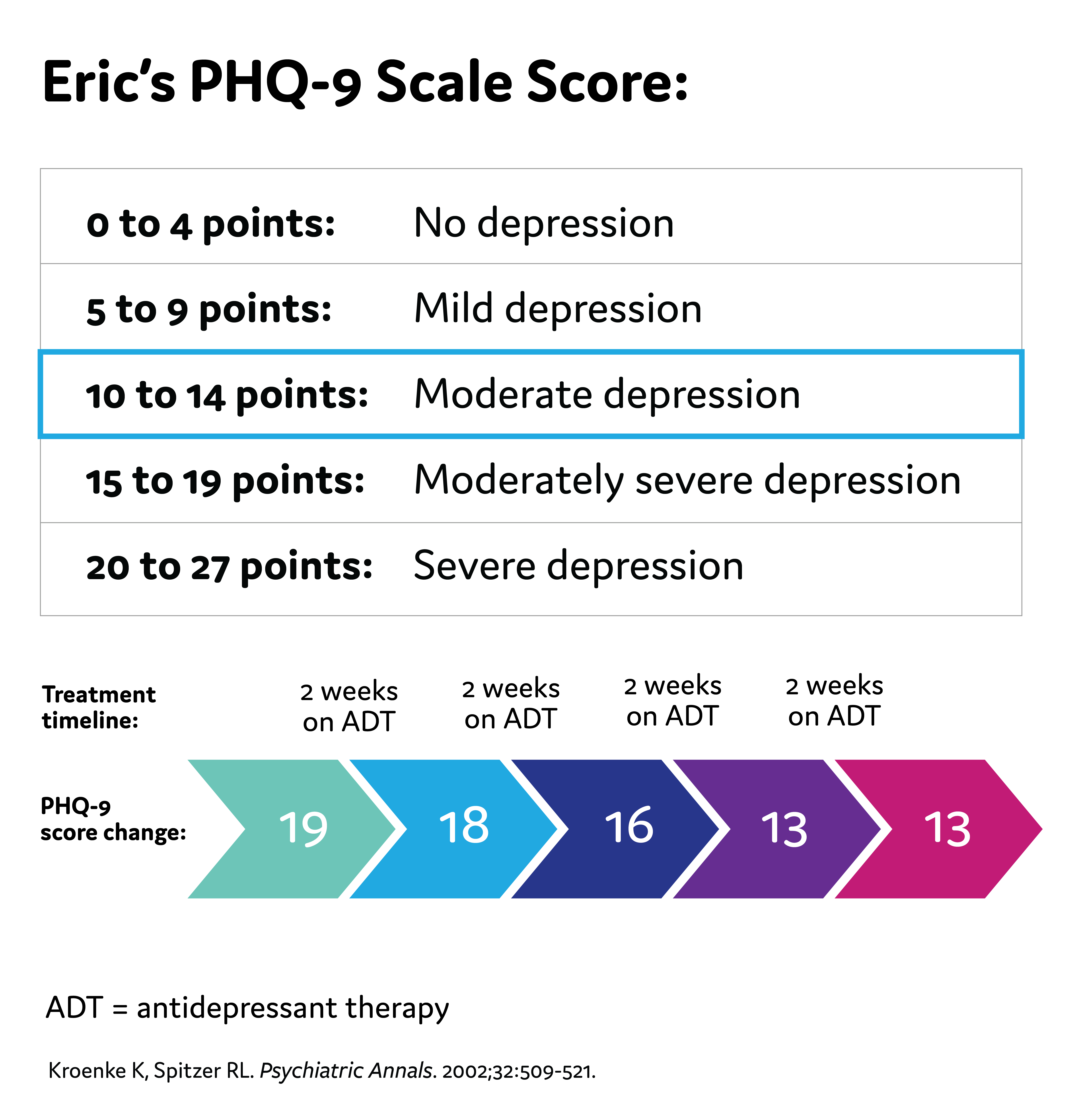
Scoring Criteria
| 0-4 | No depression |
| 5-9 | Mild depression |
| 10-14 | Moderate depression |
| 15-19 | Moderately severe depression |
| 20-27 | Severe depression |
Kroenke K, Spitzer RL. Psychiatric Annals. 2002;32:509-521.
The Quick Inventory of Depressive Symptomatology (QIDS)
- The QIDS is a 16-item, multiple-choice questionnaire in which depressive symptoms are rated on a 0-3 scale according to severity
- Items are derived from the 9 diagnostic criteria for major depressive disorder used in the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV), including sadness, loss of interest or pleasure, poor concentration or decision-making, self-outlook, suicidal ideation, lack of energy, sleep disturbance, appetite change, and psychomotor agitation
- Although the QIDS was initially developed based on DSM-IV criteria, the scale is also compatible with the DSM-5. The core criteria for MDD are consistent across these editions
Rush AJ, et al. Biol Psychiatry. 2003;54(5):573-583.
Scoring Criteria
| 0-5 | Normal |
| 6-10 | Mild |
| 11-15 | Moderate |
| 16-20 | Severe |
| ≥ 21 | Very Severe |
Bernstein IH, et al. Int J Methods Psychiatr Res. 2009;18(2):138-146.
Watch the video:
Quiz #3: Scales for MDD
Treatment Initiation and Monitoring
APA Guidelines
Eric's PHQ-9 Score
Treatment Options
American Psychiatric Association (APA) Guidelines for Treatment of MDD
1-2 weeks: Improvement from pharmacologic therapy can be seen as early as 1-2 weeks after starting treatment
2-4 weeks: Some patients may achieve improvement in 2-4 weeks
4-6 weeks: Short-term efficacy trials show antidepressant therapy appears to require 4-6 weeks to achieve maximum therapeutic effects
4-8 weeks: The APA recommends 4-8 weeks of adequate* treatment is needed before concluding that a patient is partially responsive or unresponsive to treatment *Adequate dose and duration Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
*Adequate dose and duration
Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
Watch the video:
Quiz #4: Treatment Initiation and Monitoring
Assessing for Treatment Challenges
Treatment Challenges
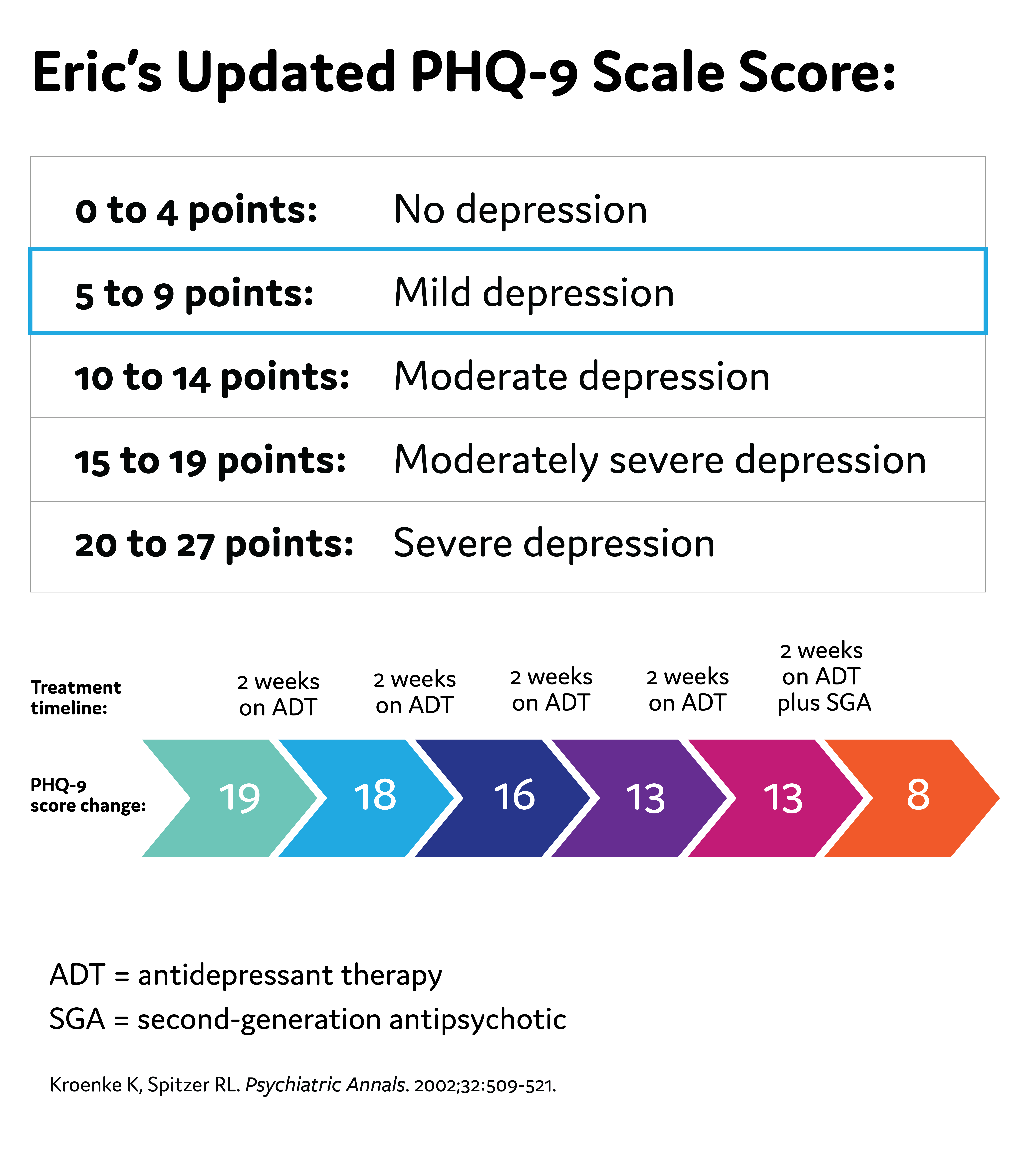
Eric's Updated PHQ-9 Score
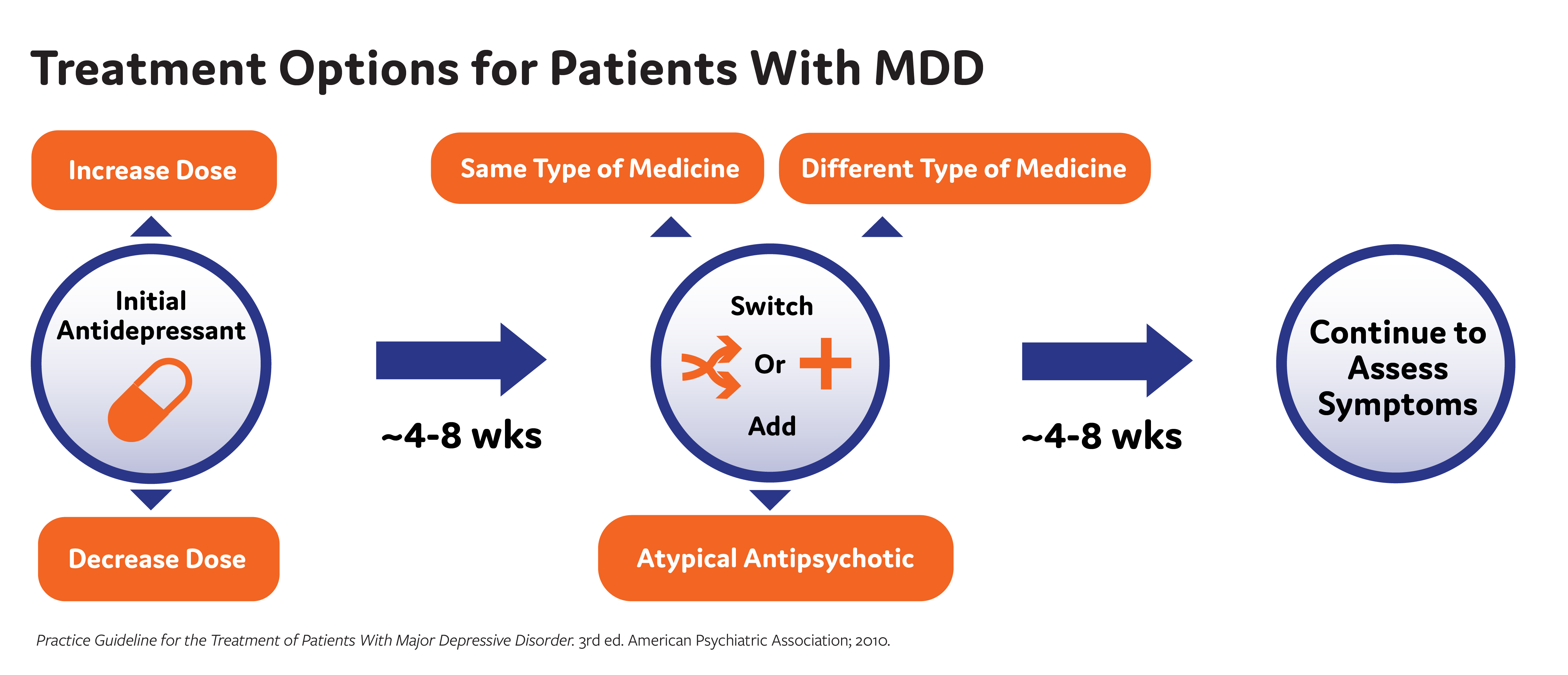
Possible Challenges to Antidepressant Therapy
- Suboptimal efficacy due to the wrong dose, inadequate length of time on the medication, or the person's individual biology not being responsive to the medication
- Unpleasant side effects of antidepressants can occur, such as weight gain, insomnia, and sexual dysfunction
- Nonadherence to the antidepressant
- As a reminder, the American Psychiatric Association (APA) recommends 4-8 weeks of adequate* treatment is needed before concluding that a patient is partially responsive or unresponsive to treatment
*Adequate dose and duration
Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
Watch the video:
Conclusion
MDD Diagnosis
Clinical Probes
Treatment Assessment
Monitoring Considerations
Factors to Consider When Making a MDD Diagnosis
- Take a thorough patient history
- Previous or current depressive episodes
- Previous or current manic or hypomanic episodes
- Family history of MDD, bipolar disorder
- Medical comorbidities
- Consider a broad differential diagnosis
Clinical Queries That Aid in Diagnosing Major Depressive Episodes
|
|
|---|---|
| DSM-5 Criteria | Clinical Queries |
| 1. Depressed mood most of the day, nearly every day | 1. Have you been experiencing persistent feelings of low mood, sadness, or hopelessness? |
| 2. Markedly diminished interest or pleasure in activities most of the day, nearly every day | 2. Have you noticed a decrease in interest or pleasure in activities that you once enjoyed? |
| 3. Significant change in weight or appetite | 3. Have your eating habits changed, either with a decrease or increase in appetite? |
| 4. Insomnia or hypersomnia | 4. Have you noticed and changes in your sleep patterns? |
| 5. Psychomotor agitation or retardation | 5. Have you felt unusually restless or fidgety, or slower than usual in your movements or speech? |
| 6. Fatigue or loss of energy | 6. Have you been feeling more tired and consistently low on energy? |
| 7. Feelings of worthlessness or excessive or inappropriate guilt | 7. Have you been struggling with feelings of low self-worth? |
| 8. Diminished ability to think or concentrate, or indecisiveness | 8. Are you finding it difficult to concentrate or think clearly? |
| 9. Recurrent thoughts of death or suicidal ideation | 9. Have you been having thoughts about death or harming yourself? |
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. American Psychiatric Association; 2013. 2. Kroenke K, et al. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613.
APA Practice Guidelines on Treatment Assessment
- Wait 4 to 8 weeks to assess treatment response to antidepressants
- In patients without adequate response, clinicians can consider changing or augmenting with a second medication
- Changes to treatment plans, such as augmenting with a second-generation antipsychotic medication, are reasonable if a patient does not have adequate improvement in 6 weeks
- Consistently follow-up with patients to assess treatment effects, adverse medication effects, and risk of self-harm
Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
APA Practice Guidelines note that the frequency of monitoring should be based on:
- Symptom severity (including suicidal ideation)
- Co-occurring disorders (including general medical conditions)
- Treatment adherence
- Availability of social supports
- Frequency and severity of side effects with medication
Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
Watch the video:

Tina Matthews-Hayes is a paid consultant for Abbvie Medical Affairs and was compensated for her time.
References
American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
- Kapfhammer HP. Somatic symptoms in depression. Dialogues Clin Neurosci. 2006;8(2):227-239.
- Bobo WV. The diagnosis and management of bipolar I and II disorders: clinical practice update. Mayo Clin Proc. 2017;92(10):1532-1551.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613.
- Smarr KL, Keefer AL. Measures of depression and depressive symptoms. Arthritis Care Res. 2011;63(S11):S454-S466. doi:10.1002/acr.20556
- Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573-583.
- Brown ES, Murray M, Carmody TJ, et al. The Quick Inventory of Depressive Symptomatology–Self-report: a psychometric evaluation in patients with asthma and major depressive disorder. Ann Allergy Asthma Immunol. 2008;100(5):433-438. doi:10.1016/S1081-1206(10)60467-X
- Liu R, Wang F, Liu S, et al. Reliability and validity of the Quick Inventory of Depressive Symptomatology-Self-Report Scale in older adults with depressive symptoms. Front Psychiatry. 2021;12:686711. doi:10.3389/fpsyt.2021.686711
- Bernstein IH, Rush AJ, Suppes T, et al. A psychometric evaluation of the clinician-rated Quick Inventory of Depressive Symptomatology (QIDS-C16) in patients with bipolar disorder. Int J Methods Psychiatr Res. 2009;18(2):138-146. doi:10.1002/mpr.2855
- Bernstein IH, Rush AJ, Trivedi MH, et al. Psychometric properties of the Quick Inventory of Depressive Symptomatology in adolescents. Int J Methods Psychiatr Res. 2010;19(4):185-194. doi:10.1002/mpr.321
- Kroenke K. Enhancing the clinical utility of depression screening. CMAJ. 2012;184(3):281-282.doi:10.1503/cmaj.112004
- Levinstein MR, Samuels BA. Mechanisms underlying the antidepressant response and treatment resistance. Front Behav Neurosci. 2014;8:208. doi:10.3389/fnbeh.2014.00208
- Haddad PM, Talbot PS, Anderson IM, McAllister-Williams RH. Managing inadequate antidepressant response in depressive illness. Br Med Bull. 2015;115(1):183-201. doi:10.1093/bmb/ldv03
This resource is intended for educational purposes only and is intended for US healthcare professionals. Healthcare professionals should use independent medical judgment. All decisions regarding patient care must be handled by a healthcare professional and be made based on the unique needs of each patient.
This is not a diagnostic tool and is not intended to replace a clinical evaluation by a healthcare provider.
Reach out to your family or friends for help if you have thoughts of harming yourself or others, or call the National Suicide Prevention Helpline for information at 800-273-8255.
ABBV-US-00976-MC, V1.0
Approved 12/2023
AbbVie Medical Affairs
Recommended on NP Psych Navigator

Clinical Article
Anhedonia and Cognitive Function in Adults With MDD: Results From the International Mood Disorders Collaborative Project
The International Mood Disorders Collaborative Project found a significant correlation between anhedonia and self-reported cognitive impairment in adults with major depressive disorder (MDD), which may help to identify individuals with MDD who are at higher risk of cognitive decline over time.

Clinical Article
Unrecognized Bipolar Disorder in Patients With Depression Managed in Primary Care: A Systematic Review and Meta-Analysis
Daveney et al explore the characteristics of patients with mixed symptoms, as compared to those without mixed symptoms, in both bipolar disorder and major depressive disorder.


