Skip to section
Introduction to Schizophrenia
What Is Schizophrenia?
Schizophrenia is a chronic psychiatric disease that severely impacts the quality of life of patients as well as their caregivers.1-3 It is a disorder of brain function that affects a person’s thoughts, feelings, and behavior.3 Symptoms can vary from one patient to another.3 In some cases, symptoms of schizophrenia can develop progressively, while in others they appear abruptly.3 Because of the complexity of schizophrenia, there can be common misconceptions about the disease.
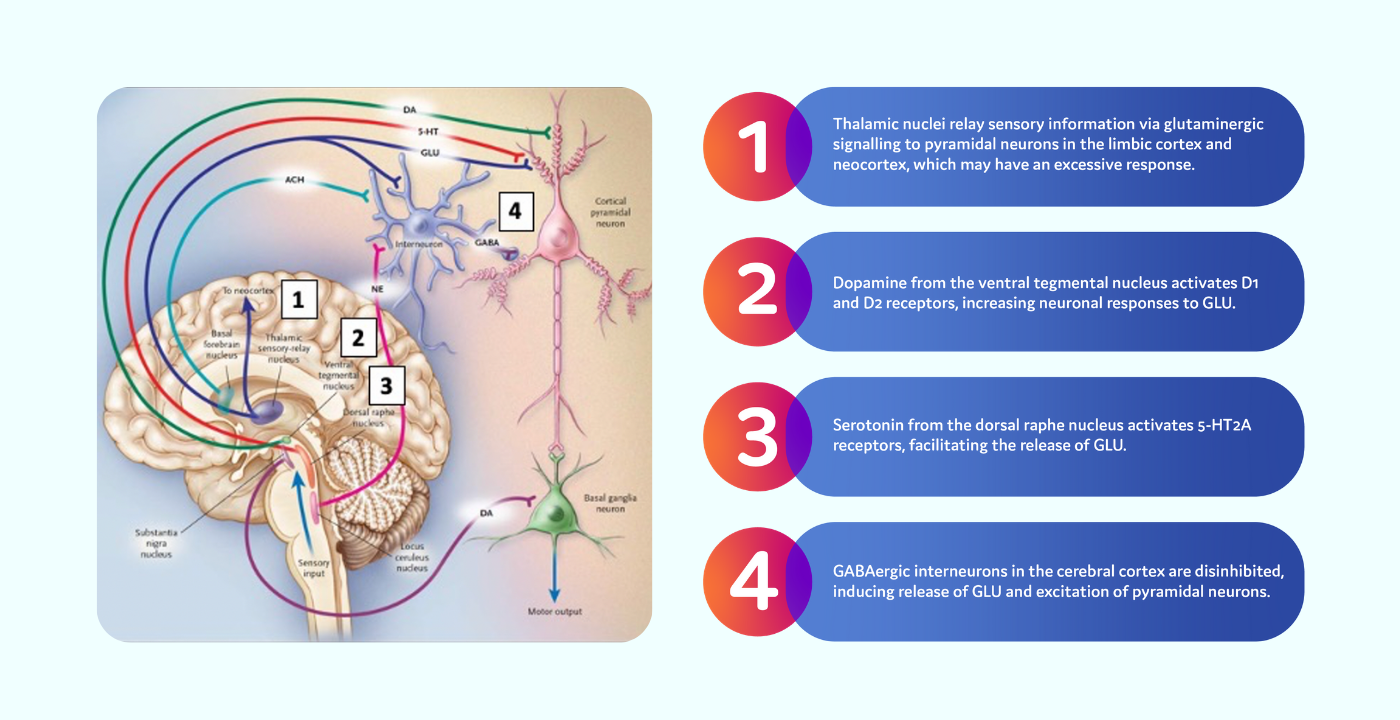
Pathophysiology of Schizophrenia
What Do We Know About the Causes?
Diagnosis
DSM-5 Diagnostic Criteria
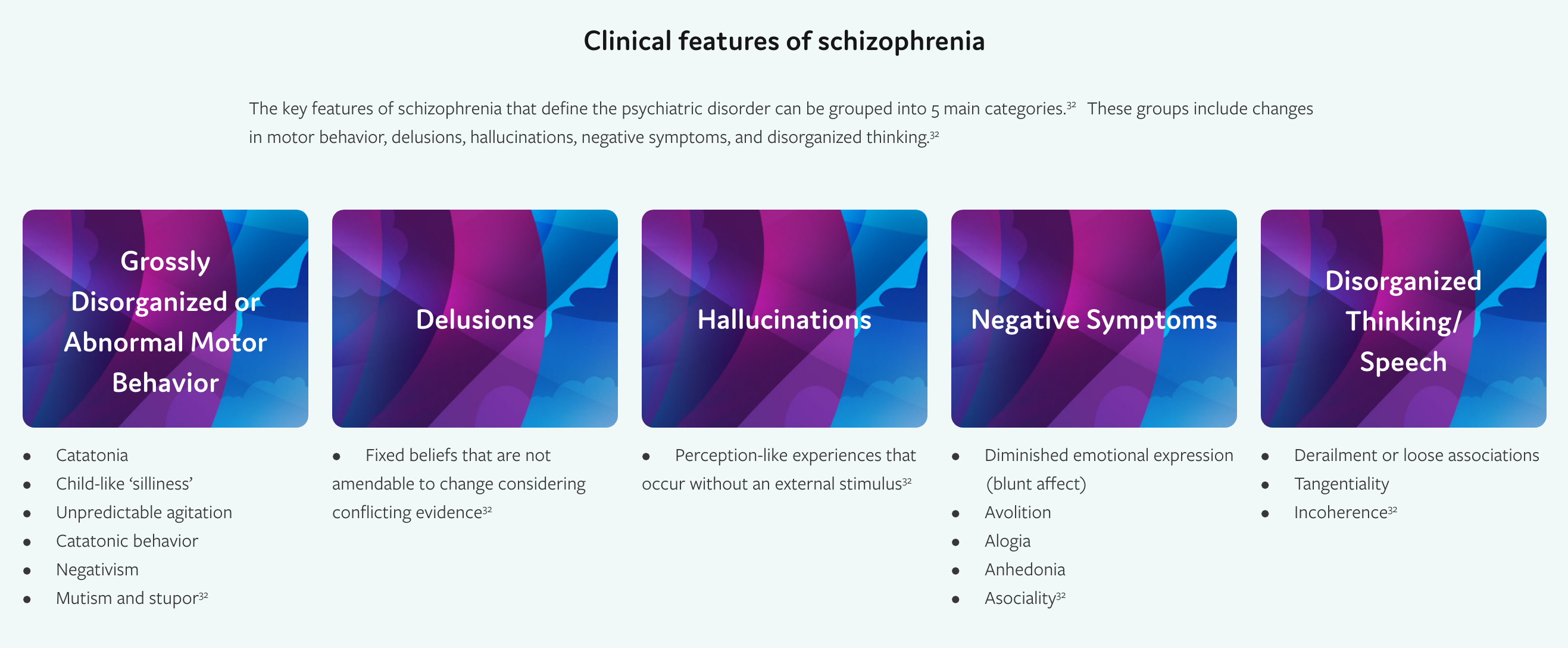
The Diagnostic and Statistical Manual, 5th Edition (DSM-5), developed by the American Psychiatric Association (APA), provides resources on the symptoms, diagnostic features, risk factors, and comorbidities associated with schizophrenia.32 While the criteria listed within the DSM-5 are used to distinguish schizophrenia, there is no single symptom that is specifically characteristic to schizophrenia.32 Every patient will differ on how clinical symptoms present.32
In order to diagnose a patient with schizophrenia, there must be continuous signs of disturbance that persist for at least 6 months and include at least 1 months of key clinical features, including 2 or more of the following:32
- Delusions
- Hallucinations
- Disorganized speech
- Grossly disorganized or catatonic behavior
- Negative symptoms
This may include prodromal or residual phases, during which only negative symptoms or attenuated symptoms are seen.32 Level of functioning in 1 or more major areas, such as work, interpersonal relations, or self-care is markedly diminished.32
Schizoaffective disorder and depressive or bipolar disorder with psychotic features must be ruled out, using the following criteria32:
- No major depressive or manic episodes occurring at the same time as active-phase symptoms; or
- If mood episodes occur at the same time as active-phase symptoms, they are present for a minority of the active and residual periods of illness
A schizophrenia diagnosis also requires ruling out that the disturbance can be attributed to the effects of a substance or another medical condition.32
In individuals with a history or autism spectrum disorder or a communication disorder with an onset in childhood, a diagnosis of schizophrenia can only be made if prominent delusions or hallucinations are present for at least 1 month (or less if successfully treated), in addition to the other required symptoms.32
Comorbidities
Depression in Patients With Schizophrenia
In the US Schizophrenia Care and Assessment Program (US-SCAP), a 3-year study including 2,327 patients with schizophrenia between July 1997 and September 2003, researchers found that 39.4% of schizophrenia patients were depressed at enrollment.42 Depression was classified as a score of ≥ 16 on the Montgomery-Asberg Depression Rating Scale (MADRS). The assessment was performed at enrollment and at 12-month intervals.42
Overall, when adjusted for age, gender, and ethnicity, depressed patients with schizophrenia were significantly more likely than non-depressed patients with schizophrenia to experience the following:42
- Use relapse-related mental health services
- Be of greater safety concern in the community
- Have more substance-related problems
- Have poorer social and family relationships
- Have poorer quality of life
Substance Use and Schizophrenia
Substance Abuse
In the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study, which analyzed the baseline prevalence of depression in 1,460 patients with schizophrenia, approximately 37% of patients had a current substance use disorder.43
Smoking Prevalence
Between 70% to 80% of patients with schizophrenia are smokers, in contrast to 20% to 30% in the general population.44
Alcohol Use Disorder
Among individuals living with schizophrenia, approximately 1 in 4 will develop alcohol use disorder in their lifetime.45
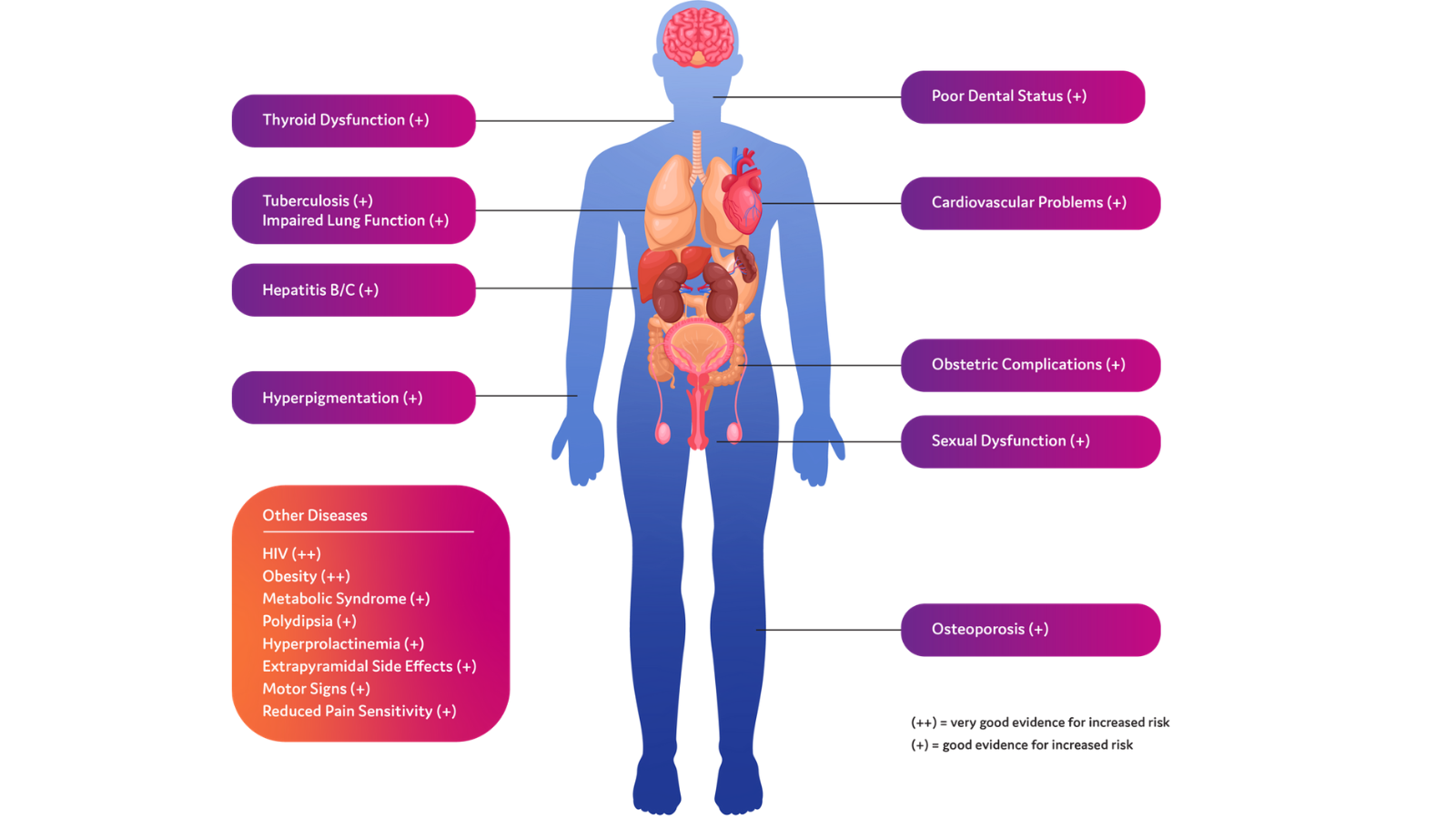
Other Comorbid Diseases in Schizophrenia
Aside from mental health and substance use disorders, schizophrenia is associated with multiple other medical comorbidities, including cardiovascular complications, obesity, thyroid dysfunction, and HIV.42,43,46
Treatment Guidelines
The treatment guidelines listed below were selected using an objective and systematic, but not exhaustive, process (see below for the methodology used). These guidelines are for educational use only. AbbVie Inc was not involved in the development of the guidelines listed below and does not endorse the use of any specific guidelines. As NP Psych Navigator is a resource for US healthcare providers, we have only included guidelines from US-based organizations. They are provided here for your convenience in alphabetical order. Healthcare providers should use their clinical judgement to determine which guidelines are appropriate for use in their clinical practice.
Agency for Health Research and Quality (AHRQ): Schizophrenia Patient Outcomes Research Team (PORT) Treatment Recommendations48
- Supporting Organizations: Agency for Health Research and Quality, the National Institute of Mental Health
- Published: 2009
- Description: The Schizophrenia Patient Outcomes Research Team (PORT) created treatment recommendations that are based primarily on empiric data, as opposed to some other clinical guidelines. The PORT treatment guidelines were created with the goal of reducing variations in care and encourage use of treatments that have strong scientific evidence. These treatment guidelines were developed using systemic reviews of literature.
American Psychiatric Association (APA): Practice Guidelines for the Treatment of Patients with Schizophrenia 202049
- Supporting Organizations: American Psychiatric Association
- Published: 2020
- Description: The APA Practice Guidelines aim to improve the quality of care and treatment outcomes for patients with schizophrenia. The guidelines were based on Treatment for Schizophrenia in Adults (McDonagh et al 2017), which was tasked by the AHRQ. The definition of schizophrenia is defined by the criteria listed in the DSM-5 manual. The guidelines focus primarily on treatment, both pharmacological and non-pharmacological, but also address assessment and patient-centered care.
- Grading: The benefits and harms of the guideline recommendations are determined by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) scale which rates recommendations by confidence that the benefits outweigh the risks. A rating of 1 indicates a recommendation, while a rating of 2 indicates a suggestion. Additionally, alphabetical ratings are assigned (A-C) to rate the strength of the supporting evidence. A grade of A indicates high strength of evidence, B indicates moderate, and C indicates low.
Texas Medication Algorithm Project (TMAP) Procedural Manual: Schizophrenia Algorithm, 200850
- Supporting Organizations: Texas Department of State and Health Services
- Published: 2008
- Description: The TMAP was developed to aid in clinical decision-making by analyzing current information regarding treatment and research data and condensing it into recommendations made based upon response, long-term safety, tolerability, and symptom remission. The algorithm addresses treatment strategies and treatment tactics. The TMAP was developed with contributions by practitioners, patients, families, and administrators.
Non-Pharmacological Management for Schizophrenia
Non-pharmacological approaches and lifestyle modifications can help patients with schizophrenia better manage their diagnoses, foster better coping skills, and improve social inclusion.51
Psychoeducation
Psychoeducation provides patients with education regarding symptom and side effect management, daily living, and relapse prevention.52 It can aid in recovery, provide resources that help patients maintain a sense of well-being, and help patients develop problem-solving skills.52 Psychoeducation has been shown to reduce mortality in patients experiencing their first episode of psychosis,49 improve global function, increase medication adherence, and improve satisfaction with treatment.49
The most important aspect of psychoeducation is that it should be tailored to the individual.52
Coordinated Specialty Care Programs
The American Psychiatric Association (APA) recommends that a patient experiencing their first episode of psychosis receive treatment at a coordinated specialty care program.49 These programs focus on family and patient education and involvement to develop personalized treatment plans and provide education and employment support.53
Cognitive Behavioral Therapy (CBT) and CBT for Psychosis (CBTp)
The APA recommends the use of CBT in patients with schizophrenia.49 CBT can improve quality of life, improve global, social and occupational function, and reduce core symptoms of illness, particularly positive symptoms.49 CBTp is cognitive behavioral therapy adapted to individuals with psychosis.49 In the setting of CBTp, patients develop their own explanations for the cognitive assumptions they have.49 These explanations are healthier and more realistic than previous assumptions; they do not perpetuate delusions or hallucinations.49
Cognitive Adaptive Training (CAT)
CAT aides in memory, focus, paying attention, and problem-solving abilities.52 This form of training encourages patients to develop lists and schedules to manage daily tasks, with a goal of allowing patients to live more independently.52
What Lifestyle Modifications Help With Schizophrenia?
The process of recovery for individuals with schizophrenia includes helping them to feel empowered to take ownership and control over their own lives.52 This can include adopting certain lifestyle modifications that can help promote and maintain wellness for those living with schizophrenia.52


.png)